Assemble the inhaler device according to the directions that come with it. For some devices, this may simply mean removing a cover; for others, it may require moving a part from one place to another. Follow the instructions that come with your spray device. Better yet, make sure you understand what your doctor told you about how to use an inhalation device before you leave her office.
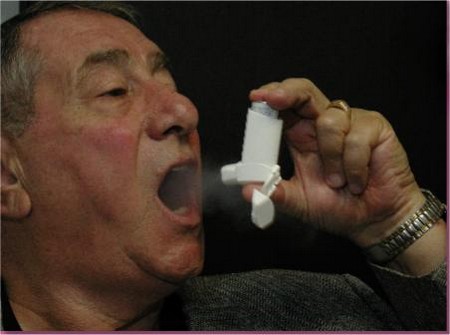
When using a spray, breathing must be through the mouth. Coordination between inhaling and triggering the spray is important. Prepare to use an inhaler by breathing out as fully as possible. Place the spray-inhaler device in your mouth, wrapping your lips around it. Squirt the device as you begin to breathe in. Breathe in as slowly and deeply as possible, then hold your breath as long as possible. Sprays are usually prescribed or labeled for two squirts to be used each time. By waiting a minute or so between squirts, the relief you get from the first dose will permit a second dose to penetrate more deeply into the lungs.

There is one unavoidable problem with the use of asthma medicine by inhalation. The very breathing difficulty that requires treatment can interfere with use of the spray medication. Let’s see why Remember that asthmatic people have a basic difficulty with exhaling, with getting the air out of the lungs. In asthma, the exhaling phase is increased, the inhaling phase decreased. But what is needed when using a spray is deep inhalation to ensure that the medication gets far enough into the airway to work on the bronchial muscles. This will be a problem with someone who spends more time breathing out than in.
Actually, most of each spray drops out of the air and comes to rest on the walls of the airway before it reaches the bronchial muscles. Some drops off in the mouth, some in the voice box, and some in the windpipe and the large bronchi before reaching the places in the smaller bronchi where it should do the most good.
There are solutions to this problem. Training the patient to breathe effectively even during an episode of asthma is a good place to start.We will discuss techniques that improve breathing for the asthmatic person. These exercises can be used to improve delivery of inhaled medicines to the places where they will work best.
A second solution, of questionable usefulness, is to use a “spacer” with the spray device that provides the medicine to be inhaled. A spacer is a container into which the measured amount of spray medication is squirted. Then, the patient can use several breaths, instead of just one, to inhale the entire dose. This is rather like offering a child medicine in a cup with a little added water so that he doesn’t have to swallow a whole tablespoonful at one time but can sip at it comfortably. There is much discussion in the medical community about the usefulness of spacers. The general opinion seems to be that, at least for patients who have trouble inhaling a spray, a spacer may help and probably won’t hurt.
A third solution is now available: one inhaler device responds to the pressure of inhaling by triggering delivery of a measured dose of its spray. When the user begins to inhale through this spray device, the inhaler automatically dispenses a dose of medication. The medicine delivered by this device is another member of the ephedrine/epinephrine family. It is called Maxair Autohaler (pirbuterol acetate).
For patients whose coordination and breathing control is not reliable, the Maxair Autohaler is a possible solution. There is also a no automatic inhaler for the same drug. Notice that both inhalers do not dispense the same amount of drug. The automatic one dispenses about half as much drug as the other.
There is another technique for using spray medicines that should be mentioned. Some sprays are recommended to be held an inch or two away from the mouth when activated. This is said to minimize absorption of the large droplets that fall out early in their trip into the respiratory tree and to permit only the small droplets to gain access into the body.
Thus far, various devices have been described that introduce measured amounts of drug into the lungs with a breath or two. Spacers have been mentioned that may provide for complete inhaling of a measured dose of the drug by permitting re-breathing until the dose is absorbed. A variation on this is the nebulizer, which is a chamber that holds a measured amount of bronchodilator drug that can be forced into the air as a “mist” (aerosol) by use of an attached air-bulb or by connection to a source of oxygen or compressed air. As the air is forced through the liquid medication, tiny particles of medicine are forced into the air, ready to be inhaled. The amount of medicine used must be carefully measured into the chamber because it will be breathed continually until all of it is absorbed.
The advantage of this re-breathing technique is that, as the bronchial tubes are dilated, continual breathing permits the medicine to penetrate deeper and deeper into the lungs. The success of this type of treatment has been demonstrated and reported in the medical books and journals. The disadvantage is that overdose is a possibility as a result of re-breathing or because of errors in measuring the original total dose. The nebulizer can also be used for certain powders used in asthma treatment. Various bronchodilator medicines are available by prescription for use by nebulizer, as are some steroids and mast cell stabilizing medicines.
Nebualizers available for purchase run from the inexpensive, simple glass chamber with an attached bulb that can be squeezed to force air through the medicine to make the aerosol to expensive mechanical devices powered by electricity or by air or oxygen from tanks. There are equalizers that heat the liquid to ensure that the size of particles is small and the temperature of the medicine will be like that of the lungs. Even ultrasound has been used to produce suitably small droplet sizes. These instruments can be equipped with face masks for small children or the usual tube for adults. These more expensive devices are usually found in hospital emergency rooms; however, some doctors prescribe them for home use for patients seriously ill with lung disease.
The various categories of available medicines are few: bronchodilators, steroids, and mast cell stabilizers. There is not much difference in the usefulness of each of the drugs within each category. One drug is as good as the next in any group. For example, among the bronchodilator sprays there is little difference in the effectiveness and safety of the metaproterenol spray (Alupent) and metaproterenol powder (Alupent). Apparently drug manufacturers have taken to selling the usefulness of their drug-delivery devices rather than the drugs themselves; they are selling the packaging rather than the medication. The choice of a device to be used by any patient will vary with each patient. Trial of several different devices and techniques may be needed before deciding what works best for an individual patient. Nor should a patient feel bound to a particular drug or device. As circumstances change, so may the drugs and the devices.